All published articles of this journal are available on ScienceDirect.
Assessment of Hepatic Steatosis in Patients with Chronic Hepatitis B Using Fibroscan and its Relation to Insulin Resistance
Abstract
Background & Aim:
Simple hepatic steatosis is a benign condition, but it may cause serious liver damage as it may lead to steatohepatitis, fibrosis and cirrhosis. The Controlled Attenuation Parameter (CAP) of fibroscan assesses hepatic steatosis. The aim of this work was to assess hepatic steatosis in patients with chronic hepatitis B infection using FibroScan and to detect its relation to insulin resistance.
Methods:
Seventy-seven patients with chronic HBV were enrolled in this study. Body mass index, complete lipid profile, fasting insulin, HOMA-IR, pelviabdominal ultrasound and fibroscan were assessed in all patients.
Results:
According to the presence of significant steatosis, seventy-seven patients enrolled in this study were divided into different groups, such as group I 47 patients (61.04%) with CHB virus infection with non-significant steatosis and group II 30 patients (38.96%) with CHB infection with significant steatosis. There was a statistically significant increase in fasting insulin and HOMA-IR in group II (p-value <0.001). CAP results ranged from 100-396 db/m with no significant difference in liver stiffness measurements in two studied groups (P value= 0.886). There was a significant positive correlation between the degree of hepatic steatosis measured by fibroscan and fasting insulin blood level, HOMA-IR, serum cholesterol and LDL. At cutoff > 222 db/m steatosis measured by fibroscan had a sensitivity of 63.33% and specificity of 82.35% for the detection of insulin resistance.
Conclusion:
In CHB infected patients, steatosis measurement by fibroscan was a strong predictor of Insulin Resistance (IR) and vice versa.
1. INTRODUCTION
Hepatitis B Virus (HBV) infection is still considered a serious universal public health problem in spite of the effective HBV vaccination programs [1]. Two billion people worldwide have been infected with HBV; 240 million people of them are chronically infected [2]. Chronic HBV infection is considered to be an important risk factor for cirrhosis and Hepatocellular Carcinoma (HCC) that can occur even in the absence of cirrhosis [3].
Simple hepatic steatosis is a benign condition that occurs when fat deposition in the liver exceeds 5% of the gross total weight of the liver, or more than 5% of hepatocytes containing fat deposits, but this benign condition may cause serious liver damage as it may develop into steatohepatitis, fibrosis and cirrhosis [4].
Liver biopsy is still considered as the ‘gold standard’ for diagnosing hepatic steatosis. However, it is associated with the risk of complications in 0.5%, and mortality in about 0.05% of the cases due to its invasive nature [5].
Liver ultrasound (US) is used frequently as an alternative non-invasive imaging diagnostic tool to assess hepatic steatosis, but it can only detect steatosis when hepatic fat content ≥ 20% [6].
The Controlled Attenuation Parameter (CAP) measured by Transient Elastography was recently introduced as a promising non-invasive quantitative test for measuring hepatic steatosis [7], as it assesses hepatic steatosis when hepatic fat content is at least 5% [8].
Insulin Resistance (IR) is the condition in which a greater than normal amount of insulin is needed to elicit a quantitatively normal response. IR was found to be linked to chronic liver disease and progression to fibrosis, cirrhosis and HCC [9]. IR can be measured by different methods (i.e. Euglycaemic clamp and modified insulin suppression test) [10], or can be calculated using equations that depend on determination of fasting plasma insulin concentrations (i.e. quantitative insulin sensitivity check index (QUICKI) and homeostatic model assessment (HOMA-IR)) [11].
Until now, the relationship between CHB infection and hepatic steatosis is still unclear [12], also its role in the occurrence of IR is still controversial [13].
The aim of this work was to assess hepatic steatosis in patients with chronic hepatitis B infection using FibroScan and to detect its relation to insulin resistance.
2. METHODS
This cross-sectional study was conducted in Tropical Medicine Department Tanta University. Seventy-seven patients who attended fibroscan examination and met our inclusion criteria in the period between 2/2017 to 6/2018 were enrolled.
Inclusion criteria included: Chronic HBV infected patients (positive HBsAg and positive quantitative PCR of HBV DNA for more than 6 months), aged > 18 years.
Exclusion criteria included: Hepatitis C virus infection, previous or ongoing alcoholism, Diabetes mellitus, and obesity body mass was calculated using the following equation: Bodyweight (kg)/height2 (m2).
Patients with body mass index > 29.9 were excluded, hepatic malignancy, use of medications associated with fatty liver disease within the past year (i.e., amiodarone, tamoxifen, methotrexate, corticosteroid, etc.).
All patients provided informed written consent and the study was approved by the Ethical Committee of Faculty of Medicine, Tanta University (the approval code 31672/07/17). All patients had code numbers to ensure the privacy of patients.
All patients were subjected to the following: Full history taking, complete physical examination, weight, height, routine laboratory investigations including (Complete blood count, liver function tests, coagulation profile and renal function test), lipid profile (including serum cholesterol, serum triglycerides, Low Density Lipoprotein (LDL) and High Density Lipoprotein (HDL), Insulin resistance calculation, Fibroscan examination and Pelvi-abdominal ultrasound.
Fasting insulin blood level (measured by the calbiotech insulin ELIZA kit) and Fasting Blood Glucose (FBG) were measured for the estimation of Homeostasis Model Assessment–insulin resistance (HOMA-IR) using the following formula:
Fasting glucose (mg/dl) x fasting insulin (µU/mL)/405.
Ultrasound of abdomen and pelvis: It was performed in Tropical medicine department using Toshiba Nemio XG apparatus with a convex probe 3.5 MHz using (B-mode) for the assessment of liver echogenicity, liver surface nodularity, liver edge, size of the liver, periportal fibrosis and narrowing of intrahepatic vessels, size of spleen and presence of other abnormal findings as ascites.
Transient Elastography: Liver stiffness measurement was performed with Fibroscan (echosens- France) 502 M probe, it was performed by experienced operators following the instructions of the manufacturer, expressing the stiffness results in Kilopascals (kPa). All measurements were performed with FibroScan (M) probe or (XL) probe. Hepatic steatosis is measured at the same session using the same probe (M probe) or (XL) probe to detect Controlled Attenuation Parameter (CAP), and data were automatically calculated concurrently with the liver stiffness measurement. CAP will be assessed only in case of a valid and reliable TE measurement. Up to 10 valid measurements were performed on each patient with a success rate of above 60% and an interquartile range/median ratio of less than 30% which were considered reliable [14].
Operators of Transient elastography were blinded to the clinical data and results of ultrasound of the patients. Transient Elastography, abdominal ultrasound, lipid profile and insulin resistance calculation were performed on the same day.
2.1. Statistical Analysis
Statistical presentation and analysis of the present study were conducted, using the mean, standard deviation, student t-test, Chi-square and Linear Correlation Coefficient by SPSS V20. ROC (receiver operator characteristic) curve was used to find out the cut-off value with the best sensitivity and specificity to assess the validity of certain variables. Data were presented as the mean ± standard deviation (SD). A p-value of less than or equal to 0.05 was considered statically significant, while p-value less than 0.01was considered highly significant.
3. RESULTS
Seventy-seven (77) patients were enrolled and categorized into two groups according to steatosis degree measured by Fibroscan (Fig. 1).
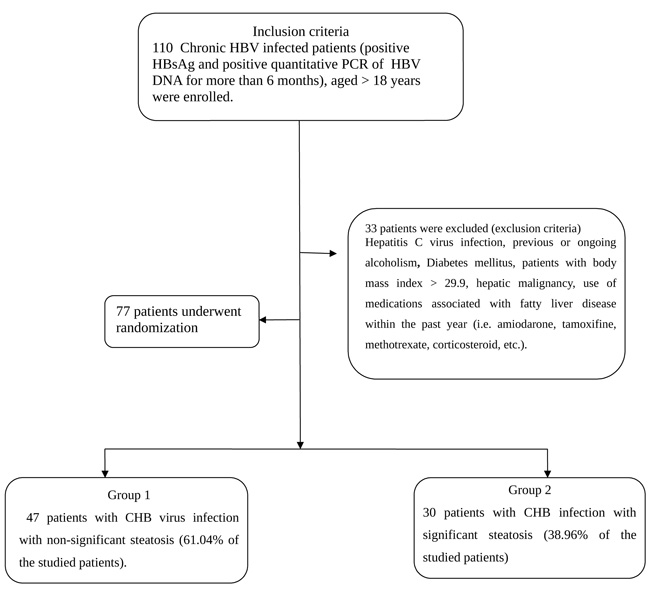
Group 1: 47 patients with CHB virus infection with non-significant steatosis CAP values > 258 (61.04% of the studied patients); Group 2: 30 patients with CHB infection with significant steatosis CAP values ≥ 258 (38.96% of the studied patients).
There were no statistical differences between the studied groups regarding age, sex, liver function tests, complete blood picture, prothrombin time, serum creatinine level, fasting blood sugar level, and quantitative PCR of HBV DNA, BMI, cholesterol, triglycerides, HDL, LDL, and liver stiffness measured by Fibroscan (Table 1).
There was a statistically significant difference between two studied groups regarding fasting insulin and HOMA-IR as they were significantly higher in the second group (17.648±6.213 vs. 23.299±6.367) and (3.495±1.056 vs. 5.133±1.177) respectively (p-value <0.001) (Table 2).
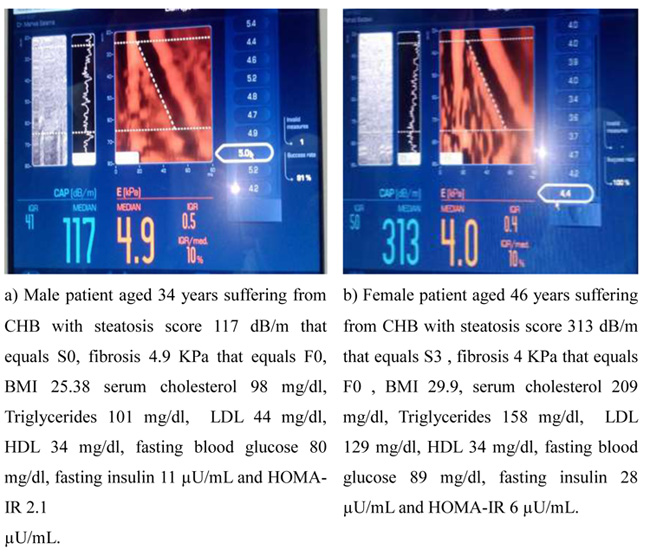
Fibroscan examination: liver stiffness measures ranged from 2.8-29.9KPa, with no significant difference between two studied groups (P value= 0.886), while CAP results ranged from 100-396 db/m (Fig. 2a, b).
Ultrasound examination for qualitative detection of liver echogenicity: There was a statistically significant difference between two studied groups as the liver appeared bright in 34.04% of the patients in group 1 (16 patients of 47 patients) vs. 83.33% in group 2 (25 patients of 30 patients) (P-value <0.001) (Table 3).
Correlations among hepatic steatosis measured by Fibroscan and different parameters: There was a significant positive correlation between the degree of hepatic steatosis measured by Fibroscan and: Fasting insulin blood level (r = 0.460/ P value < 0.001), HOMA-IR (r = 0.650/ P value < 0.001), serum cholesterol (r=0.281/ P value = 0.013) and LDL (r = 0.274/ P value = 0.016) (Table 4).
An ROC curve analysis was performed to set a cutoff of fasting insulin and HOMA IR for the detection of steatosis. At cutoff < 23, fasting insulin had a sensitivity of 63.33% and specificity of 80.85% for the detection of steatosis (AUC 0.759). While; at cutoff < 4.7 HOMA-IR had a sensitivity of 80% and specificity of 93.62% for the detection of steatosis (AUC 0.88) (Table 5).
| - | Steatosis db/m | T-test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non Significant | Significant | t | P value | ||||||||
| Age Years |
Range | 18 | - | 58 | 26 | - | 57 | 0.019 | 0.985 | ||
| Mean ±SD | 38.511 | ± | 10.43 | 38.467 | ± | 8.553 | |||||
| BMI (Kgs/m2) |
Range | 20 | - | 29.9 | 20.3 | - | 29.9 | -0.356 | 0.723 | ||
| Mean ±SD | 25.894 | ± | 2.864 | 26.135 | ± | 2.926 | |||||
| Hemoglobin (g/dl) | Range | 9.5 | - | 16.3 | 10 | - | 17 | 0.716 | 0.476 | ||
| Mean ±SD | 13.196 | ± | 1.751 | 12.887 | ± | 1.989 | |||||
| Platelet/ cmm (103) | Range | 119 | - | 348 | 100 | - | 533 | -1.332 | 0.187 | ||
| Mean ±SD | 193.255 | ± | 49.156 | 214.233 | ± | 88.965 | |||||
| WBCs /mm3 | Range | 3.7 | - | 14 | 3 | - | 12 | 0.797 | 0.428 | ||
| Mean ±SD | 7.450 | ± | 2.769 | 6.963 | ± | 2.337 | |||||
| Total bilirubin (mg/dl) | Range | 0.2 | - | 2.2 | 0.3 | - | 1.4 | -0.320 | 0.750 | ||
| Mean ±SD | 0.827 | ± | 0.372 | 0.853 | ± | 0.283 | |||||
| ALT (U/l) | Range | 6 | - | 67 | 7 | - | 72 | -0.255 | 0.8 | ||
| Mean ±SD | 26.979 | ± | 12.293 | 27.8 | ± | 15.891 | |||||
| AST (U/l) | Range | 8 | - | 70 | 6 | - | 84 | -0.510 | 0.611 | ||
| Mean ±SD | 27.404 | ± | 13.041 | 29.167 | ± | 17.173 | |||||
| Serum albumin (g/dl) | Range | 3.4 | - | 5.3 | 3.2 | - | 5.1 | -0.088 | 0.930 | ||
| Mean ±SD | 4.152 | ± | 0.401 | 4.161 | ± | 0.509 | |||||
| INR | Range | 1 | - | 1.5 | 1 | - | 1.2 | 1.520 | 0.133 | ||
| Mean ±SD | 1.054 | ± | 0.097 | 1.025 | ± | 0.046 | |||||
| Prothrombin time (seconds) | Range | 12 | - | 19 | 12 | - | 16 | 0.813 | 0.419 | ||
| Mean ±SD | 13.594 | ± | 1.583 | 13.250 | ± | 2.120 | |||||
| Serum creatinine (mg/dl) | Range | 0.02 | - | 1.3 | 0.05 | - | 1.5 | 0.086 | 0.931 | ||
| Mean ±SD | 0.736 | ± | 0.328 | 0.728 | ± | 0.435 | |||||
| Bl urea (mg/dl) | Range | 12 | - | 38 | 12 | - | 33 | ||||
| Mean ±SD | 21.404 | ± | 7.660 | 21.500 | ± | -0.056 | |||||
| PCR HBV DNA (IU/ml) | Range | 25 | - | 144000 | 20 | - | 5600000 | -1.440 | 0.154 | ||
| Mean ±SD | 55310.511 | ± | 238801.731 | 298645.700 | ± | 1123594.993 | |||||
| FBG (70-110 mg/dl) |
Range | 71 | - | 113 | 69 | - | 105 | 0.458 | 0.648 | ||
| Mean ±SD | 888.77 | ± | 11.088 | 87.67 | ± | 8.84 | |||||
| Cholesterol (mg/dl) | Range | 98 | - | 317 | 111 | - | 248 | -1.320 | 0.191 | ||
| Mean ±SD | 181.957 | ± | 45.943 | 194.667 | ± | 32.276 | |||||
| Triglycerides (mg/dl) | Range | 64 | - | 188 | 71 | - | 173 | -0.868 | 0.388 | ||
| Mean ±SD | 120.362 | ± | 32.774 | 127.133 | ± | 34.350 | |||||
| HDL (mg/dl) | Range | 23 | - | 76 | 28 | - | 70 | 0.190 | 0.850 | ||
| Mean ±SD | 47.532 | ± | 12.918 | 46.967 | ± | 12.386 | |||||
| LDL (mg/dl) |
Range | 29 | - | 247 | 39 | - | 178 | -1.769 | 0.081 | ||
| Mean ±SD | 101.319 | ± | 47.142 | 119.033 | ± | 34.943 | |||||
| Liver stifness (KPa) | Range | 2.8 | - | 29.9 | 3.4 | - | 17.6 | 0.144 | 0.886 | ||
| Mean ±SD | 6.989 | ± | 4.621 | 6.843 | ± | 3.849 | |||||
| Sex | - | Chi-Square | |||||||||
| - | N | % | N | % | X2 | P-value | |||||
| Male | 34 | 72.34 | 20 | 66.67 | 0.281 | 0.596 | |||||
| Female | 13 | 27.66 | 10 | 33.33 | |||||||
| - | Steatosis (dB/m) | T-Test | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Significant | Significant | t | P-value | ||||||
| Fasting insulin (µU/mL) |
Range | 4.86 | - | 28.3 | 4.86 | - | 30.4 | -3.855 | <0.001* |
| Mean ±SD | 17.648 | ± | 6.213 | 23.299 | ± | 6.367 | |||
| HOMA-IR (µU/mL) |
Range | 1.1 | - | 6 | 1.04 | - | 6 | -6.346 | <0.001* |
| Mean ±SD | 3.495 | ± | 1.056 | 5.133 | ± | 1.177 | |||
| Liver Echogenicity by Ultrasound | Steatosis (dB/m) | Chi-Square | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-Significant | Significant | Total | ||||||
| N | % | N | % | N | % | X2 | P-value | |
| Normal | 31 | 65.96 | 5 | 16.67 | 36 | 46.75 | 17.871 | <0.001* |
| Bright | 16 | 34.04 | 25 | 83.33 | 41 | 53.25 | ||
| Total | 47 | 100.00 | 30 | 100.00 | 77 | 100.00 | ||
| Correlations | ||
|---|---|---|
| - | Steatosis (dB/m) | |
| R | P-value | |
| PCR HBV DNA (IU/ml) | 0.064 | 0.583 |
| Fasting insulin (µU/mL) | 0.460 | <0.001* |
| HOMA-IR (µU/mL) | 0.650 | <0.001* |
| Age (years) | 0.005 | 0.969 |
| BMI (Kg/m2) | 0.150 | 0.193 |
| Hb (g/dl) | 0.058 | 0.615 |
| Platelet (×103/cmm) | 0.082 | 0.477 |
| TLC (cells/mm3) | -0.093 | 0.419 |
| Creatinine (mg/dl) | -0.014 | 0.902 |
| B. Urea (mg/dl) | -0.017 | 0.887 |
| TB mg/dl) | -0.046 | 0.690 |
| ALT U/l | -0.096 | 0.409 |
| AST U/l | 0.014 | 0.907 |
| S. albumin (g/dl) | -0.013 | 0.907 |
| INR | -0.170 | 0.140 |
| PT (seconds) | -0.048 | 0.679 |
| Fibrosis (KPa) | -0.099 | 0.394 |
| Cholesterol (mg/dl) | 0.281 | 0.013* |
| Triglycerides(mg/dl) | 0.154 | 0.181 |
| HDL(mg/dl) | 0.010 | 0.931 |
| LDL(mg/dl) | 0.274 | 0.016* |
| Fasting glucose | -0.0138 | 0.907 |
| - | Cutoff | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|---|
| Fasting insulin (µU/mL) |
>23 | 63.33 | 80.85 | 67.9 | 77.6 | 75.9% |
| HOMA-IR (µU/mL) |
>4.7 | 80.00 | 93.62 | 88.9 | 88.0 | 88% |
| - | Cutoff | Sensitivity | Specificity | PPV | NPV | Accuracy |
| Steatosis | >222 | 63.33 | 82.35 | 92.7 | 38.9 | 67.53% |
At cutoff < 222 db/m steatosis measured by fibroscan had a sensitivity of 63.33% and specificity of 82.35% for the detection of insulin resistance (AUC 0.67) (Table 6).
4. DISCUSSION
There was no significant difference regarding age and sex between our two studied groups in accordance with Baclig et al., (2018), who reported no significant correlation between the age and steatosis in CHB infected patients [15]. In contrast, Rastogi et al., (2011) and Lin et al., (2007) concluded that older CHB infected patients were more liable to have steatosis [16, 17].
Moreover, Cheng et al., (2013) found that males tend to have a higher risk of fatty liver before the age of 50 than females due to more common accumulation of visceral fat in males, while in females estrogen plays a protective role against visceral fat accumulation and decreases insulin resistance before the age of 50. These differences in results may be due to different methods of assessment of steatosis as they used liver biopsy and abdominal Ultrasound for the detection of steatosis [18].
In regard to laboratory tests, there was no significant difference between the two studied groups. On the contrary, Demir et al., (2007) and Joo et al., (2017) concluded that ALT was higher in patients with CHB suffering from steatosis [19, 20].
The effect of viral load using quantitative PCR for HBV DNA on the development of steatosis has also been studied but there was no statistically significant difference between the two studied groups; it was similar to previous studies [9, 21]. On the other hand, Rastogi et al., (2011) and Enomoto et al., (2016) documented that CHB infected patients without steatosis have higher PCR for HBV DNA [16, 22].
Despite there were no statistically significant differences regarding serum cholesterol, triglycerides, Low-density Lipoproteins (LDL) and high-density lipoproteins (HDL) between the two studied groups. Serum cholesterol and LDL showed a positive correlation with hepatic steatosis measured by Fibroscan. Similarly, Baclig et al., (2018) and Tirosh O., (2018) reported that serum cholesterol correlates with the occurrence of hepatic steatosis [15, 23]. While other studies reported that triglycerides tend to be higher in patients with steatosis [16, 24, 25].
As regards Fasting Blood Glucose (FBG) there was no significant difference between the two studied groups, also there was no correlation with steatosis measured by Fibroscan. This was in agreement with the results obtained by Rastogi et al., (2011) [16], while Cheng et al., (2013) stated that FBG tends to be higher in CHB infected patient with steatosis than those without steatosis, these differences may be due to using different tools in the assessment of steatosis (Ultrasound vs. Fibroscan) and they included diabetic patients in their study [18].
On the other hand, there was a positive correlation between insulin resistance and FBG.
Fasting insulin and insulin resistance calculated by HOMA-IR were significantly higher in patients in the second group and there was a positive correlation between the degree of hepatic steatosis measured by Fibroscan for all patient groups and fasting insulin level. These results were in agreement with previous studies [9, 26, 27].
There was also a positive correlation between fasting insulin and cholesterol, triglycerides and LDL. This was in agreement with prior studies [28, 29].
After ROC curve analysis, cutoff values with the best sensitivity and specificity had been chosen. At cutoff > 4.7, HOMA-IR had a sensitivity of 80% and a specificity of 93.62% for the detection of steatosis. Similar to our study, Ubiña-Aznar et al., (2017) concluded that at cut-off 4.9 HOMA-R had 100% sensitivity and 67.9% specificity for the detection of steatosis. However, this study was conducted on 94 non-CHB infected children to determine the factors associated with increased risk for steatosis [30].
To our knowledge, this is the first study to determine the cutoff value for Steatosis degree detected by Fibroscan for the detection of insulin resistance in CHB patients and it was found that at cutoff 222db/m hepatic steatosis had a sensitivity of 63.33% and a specificity of 82.35% for detecting insulin resistance.
There was no significant difference between the two studied groups regarding the degree of liver fibrosis measured by Fibroscan. This was supported by data revealed by Zhang et al., (2019) who performed liver biopsy, Transient Elastography (TE) and Ultrasound for the assessment of steatosis and fibrosis, and concluded that there was no significant correlation between fibrosis and steatosis, and they added that Fibroscan is more accurate than other two methods in the assessment of steatosis and fibrosis [31]. Several previous studies had concluded the same results [9, 32-36].
All our patients had ultrasound examinations for qualitative assessment of liver steatosis and it was found that a statistically significant difference regarding liver echogenicity detected by ultrasound as 83.33% of our patients in the second group had bright liver. This was in agreement with the study documented by Li et al., (2018) [37].
One of the limitations of our study is the small sample size, also healthy volunteers in our study were not included, so further studies are needed to improve the validity of our results.
CONCLUSION
In conclusion, steatosis measured by Fibroscan in CHB infected patients is a strong predictor of Insulin Resistance (IR) and vice versa. In addition, liver echogenicity detected by ultrasound in CHB patients can be used as a predictor of liver steatosis.
LIST OF ABBREVIATIONS
| HBV | = Hepatitis B Virus |
| HCC | = Hepatocellular Carcinoma |
| US | = Ultrasound |
| CAP | = Controlled Attenuation Parameter |
| IR | = Insulin Resistance |
| QUICKI | = Quantitative Insulin Sensitivity Check Index |
| HOMA-IR | = Homeostatic Model Assessment |
| CHB | = Chronic Hepatitis B |
| LDL | = Low Density Lipoprotein |
| HDL | = High Density Lipoprotein |
| BMI | = Body Mass Index |
| FBG | = Fasting Blood Sugar |
| ALT | = Alanine Aminotransferase |
| AST | = Aspartate Aminotranfrase |
| WBCs | = White Blood Cells |
| TE | = Transient Elastography |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethical Committee of Faculty of Medicine, Tanta University (the approval code 31672/07/17).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All patients provided informed written consent.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


